Thank you for using our online appointment, the appointment service you have chosen is not yet confirmed. Our customer service will contact you via email or phone within 2 working days to confirm your appointment details.

What is Glaucoma?
Glaucoma is a major cause of blindness in Hong Kong. Among every hundred adults over the age of forty, three or more are likely to develop glaucoma. Early diagnosis of glaucoma can prevent vision loss and blindness.
The primary cause of permanent blindness
Early-stage glaucoma may not have obvious symptoms and is often overlooked by patients. By the time patients realize there is a problem with their eyes, the condition is often already severe, thus glaucoma is also known as the "invisible vision killer". Glaucoma can lead to permanent blindness, but if diagnosed and treated early, it can prevent vision damage. Those over forty years old, and those with high-risk factors, should have an annual eye check-up to help diagnose early-stage glaucoma and prevent deterioration.
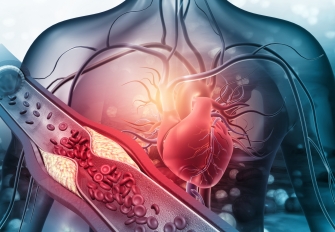
Causes of Glaucoma
There is a transparent fluid continuously flowing within the eyeball called the "aqueous humor". Similar to a sink with a faucet left running, if there is an overproduction of aqueous humor or a blockage in drainage, the pressure within the eyeball can increase, damaging the eye and optic nerve, leading to a decrease in vision or even blindness. Senior ophthalmologists, through clinical examination and advanced testing techniques, can effectively diagnose glaucoma in patients.
Classification of Glaucoma
Glaucoma can be classified into acute or chronic, congenital or acquired, primary or secondary, and normal-tension or high-tension, depending on different causes or conditions.
- Acute Glaucoma
Acute glaucoma occurs very suddenly. Patients may suddenly experience blurred vision, see a rainbow halo around lights, have red and painful eyes, and even experience headaches, nausea, and vomiting. This is an ophthalmic emergency that requires immediate medical attention. The eye pressure should be reduced as soon as possible with oral medication, injections, and eye drops, followed by laser or other surgical treatments.
- Chronic Glaucoma
Chronic glaucoma has no obvious symptoms in the early stage. Patients' vision gradually declines and their field of vision gradually narrows. Because the symptoms of chronic glaucoma are not obvious, many patients don't realize they've lost a significant portion of their vision until the disease is severe, and the situation cannot be reversed. Hence, glaucoma is also known as the "sneak thief of sight".
- Congenital and Acquired Glaucoma
Although many glaucoma patients are over forty years old (acquired), some babies are born with abnormal aqueous humor drainage systems, leading to congenital glaucoma. Babies with congenital glaucoma often show symptoms of light sensitivity and excessive tearing, and their eyeballs are larger than normal.
- Primary and Secondary Glaucoma
Primary glaucoma generally refers to glaucoma that is not caused by other diseases. Secondary glaucoma is caused by other eye or systemic diseases, such as mature cataracts, uveitis, ocular tumors, diabetic eye disease, or long-term use of steroid eye drops. To treat secondary glaucoma, the disease causing the glaucoma must be addressed first.
- Normal-tension Glaucoma
Some patients have glaucoma despite normal intraocular pressure. This is because the pressure that their optic nerves can withstand is lower than that of a normal person, leading to what is known as "normal-tension glaucoma". Therefore, a more detailed examination is often required for diagnosis.
- High-tension Glaucoma
The general cause of glaucoma is high intraocular pressure, which damages the optic nerve in the eye, leading to a decline in vision and visual field defects.
Chronic glaucoma has no obvious symptoms in the early stage, and acute glaucoma has the following symptoms:
In the clinical diagnosis, patients will undergo a series of eye check-up, including vision tests, visual field tests, fundus examinations, and eye pressure measurements. Ophthalmologists will also make diagnoses based on the patient's past medical history and family history.
Common eye check-up include:
- Eye pressure test
- Visual field tests
- Slit lamp examination
- Gonioscopy
- Assessment of the extent of optic nerve damage
- Examination of the aqueous humor outflow
Treatment of Glaucoma
The goal of glaucoma treatment is to effectively control intraocular pressure, prevent or slow the progression of glaucoma, protect and maintain the patient's optic nerve tissue and its function, and reduce further damage to the optic nerve. Treatment methods include medication (eye drops or oral medication), laser treatment, or glaucoma surgery. Among these, minimally invasive options are now available for laser treatment and surgery.
Early detection of glaucoma is crucial! Ninety percent of patients will not go blind.
The Operation / Procedure
The procedure is usually performed under local anaesthesia. The doctor gives medications to numb the procedure site and you will remain awake, general anaesthesia may be used in special circumstances.
- To increase the drainage of intraocular fluid:
- Trabeculectomy
The procedure is to create a small drainage site in the wall of the eyeball to facilitate the outflow of intraocular fluid in a controlled manner and the aim is to prevent further deterioration of visual functions and ocular damage caused by the raised intraocular pressure.
- Non penetrating glaucoma surgery
A similar procedure as trabeculectomy but a very thin layer of tissue is kept behind. A piece of collagen implant may be used to maintain the patency of the drainage site.
- Glaucoma Implant
Made of inert material like special plastic or silicone, the implant usually composed of a tube to drain the fluid out.
- Minimally invasive glaucoma surgery, MIGS
- To decrease the production of fluid inside the eye:
- laser or cryo-therapy
To destroy the tissue producing the fluid
Before the Operation / Procedure
- You should continue to use the usual eye drops or medications unless directed by doctor otherwise.
- Inform your doctor if you have other systemic disease such as hypertension, stroke, heart disease, diabetes or take western medication (especially blood thinners like Aspirin or Warfarin), traditional Chinese medicine or healthy supplements on a regular basis.
After the Operation / Procedure
- Keep eye patch or eye shield on if any as directed by doctor.
- Use eye drops or eye ointment as prescribed, those medications will help to prevent infection and inflammation.
- Keep the wound clean, avoid eye rubbing.
- Do not expose your eye to water such as showering or swimming.
- Avoid washing your hair during the first week after the operation in order to prevent dirty water getting into the eye causing infection.
- Wear clothes with buttons and not pullovers so as to avoid the clothes coming in contact with the operated eye causing infection.
- Have light on at night time when you go to toilet in order to prevent falls as you may not be accustomed with one eye being patched after the operation.
- Avoid unnecessary straining after surgery. If you have constipation, take liberal amounts of vegetables and fruits to alleviate your constipation if there is no contraindication.
- You may be recommended to sleep on the side opposite to the operated eye and protect the operated eye during sleep by wearing an eye shield.
Follow-up
- For several weeks following the surgery, your eye doctor will observe your eye closely and examine you frequently. During this time period, the eye pressure has not yet stabilized. Avoid lifting heavy objects, bending or straining.
- You must follow instructions strictly on taking medications and see the doctor as scheduled.
- Eyeball pressure and signs of recurrence will be monitored. You may need to restart eye drops to control glaucoma if the pressure shoots up again or even another operation if the pressure is uncontrolled.
- If you have any excessive bleeding, severe pain, fever or signs of wound infection such as redness, swelling or large amounts of foul-smelling discharge coming from your eye, see your doctor immediately or attend the nearby Accident and Emergency Department.